
I. Introduction
A. Importance of understanding the menstrual cycle
A normal and important process that takes place in the female reproductive system is the menstrual cycle (also known as period). It plays a crucial role in preparing the body for potential pregnancy and maintaining overall reproductive health. You can monitor your fertility, identify any anomalies, manage any pain or symptoms related to menstruation, and make educated choices about your health by being aware of your menstrual cycle.
B. Purpose of the guide
This comprehensive guide aims to provide a detailed, friendly, and straightforward explanation of the menstrual cycle. It will cover the different phases, hormonal changes, common concerns, and self-care tips. By the end of this guide, you should know a lot about your period and feel like you can take care of your reproductive health.
II. What is the Menstrual Cycle?
A. Definition and overview
A woman’s body undergoes a series of hormonal and physiological changes during her menstrual cycle in order to be ready for a prospective pregnancy. The menstrual cycle begins on the first day of bleeding and lasts until the day before the start of the subsequent period. An egg must mature and be released, and the uterine lining must alter in order to enable the potential implantation of a fertilized egg.
B. Average cycle length
The menstrual cycle lasts 28 days on average, however it can last between 21 and 35 days for adults and between 21 and 45 days for teenagers. It’s important to note that each woman’s cycle may differ and that variations in cycle length are expected, especially during the first few years after menstruation begins or as a woman approaches menopause.
C. Hormones involved in the menstrual cycle
A complicated interaction of hormones released by the brain and ovaries controls the menstrual period. These hormones include:

Estrogen
This hormone is in charge of both the maturation of the egg inside the ovary and the development and thickness of the uterine lining. During the follicular phase, estrogen levels increase and reach their peak just before ovulation.
Progesterone
Produced by the corpus luteum after ovulation, progesterone prepares the uterus for the potential implantation of a fertilized egg and helps maintain pregnancy if conception occurs. Progesterone levels rise during the luteal phase and drop if no pregnancy occurs, leading to menstruation.
Follicle-stimulating hormone (FSH)
The ovarian follicles, which house immature eggs, are stimulated to grow and develop by the hormone FSH, which is released by the pituitary gland in the brain. FSH levels are highest at the beginning of the follicular phase.
Luteinizing hormone (LH)
LH, which is also made by the pituitary gland, causes ovulation, or the release of the mature egg from the ovary. LH levels surge approximately 24-48 hours before ovulation, creating what’s known as the “LH surge.”
III. Phases of the Menstrual Cycle
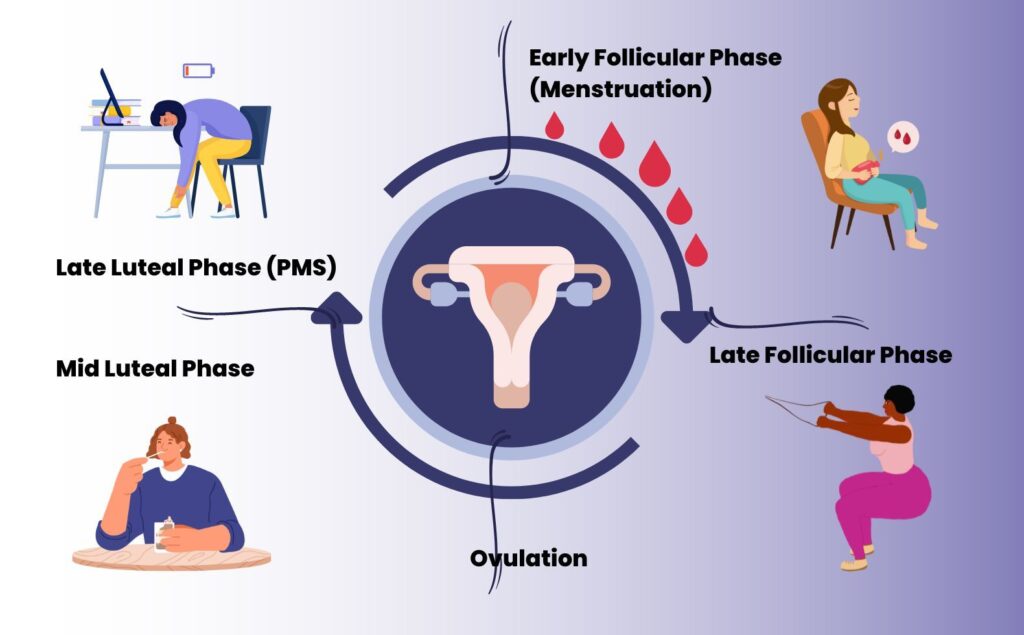
A. Menstrual phase
Shedding of the uterine lining
The first day of menstruation marks the start of the monthly period, which lasts until the bleeding ceases. Due to a decline in estrogen and progesterone levels, the endometrium, the thickened lining of the uterus, sheds during this phase. This shedding results in menstrual bleeding, typically lasting 3 to 7 days.
Duration and symptoms
The duration and symptoms of the menstrual phase may vary among women. Headaches, bloating, exhaustion, mood changes, and cramps are typical symptoms. More severe symptoms, such as persistent discomfort or heavy bleeding, may also be experienced by some women and necessitate medical treatment.
B. Follicular phase
Development of follicles
The first day of menstruation marks the start of the follicular phase, which lasts until ovulation. The pituitary gland produces FSH at this stage, which promotes the development of many ovarian follicles. There are immature eggs in each follicle, but only one matures and releases an egg during ovulation.
Hormonal changes
The uterine lining thickens to prepare for a potential pregnancy while the follicles grow and release estrogen. Eventually, the rising estrogen levels cause LH to release, which results in ovulation.
C. Ovulation
Release of the mature egg
Ovulation is the release of the mature egg from the dominant follicle in the ovary. It usually occurs around day 14 of a 28-day cycle, but the exact timing can vary among women. The LH surge causes ovulation, which results in the release of the egg into the fallopian tube where it can be fertilized by sperm.
Signs and symptoms
Some women may experience mild symptoms during ovulation, such as lower abdominal pain (mittelschmerz), increased libido, or changes in cervical mucus. Cervical mucus tends to become clear, slippery, and stretchy around ovulation, resembling raw egg whites. This change in consistency helps sperm travel more easily toward the egg.
D. Luteal phase
Formation of the corpus luteum
Immediately after ovulation, the luteal phase starts. The remains of the dominant follicle develop into the corpus luteum, a structure that makes progesterone, at this stage. This hormone helps to maintain the thickened uterine lining and support a potential pregnancy.
Hormonal changes
The corpus luteum disintegrates if the egg is not fertilized, lowering progesterone and estrogen levels. This hormone decrease causes the uterine lining to slough, which causes menstruation and the beginning of a new menstrual cycle.
E. Charting menstrual cycle phases

Understanding the various stages of your menstrual cycle can aid in ovulation prediction, fertility monitoring, and the detection of any possible anomalies. Some techniques for charting the phases of your menstrual cycle include:
Calendar method
Use a calendar or app to record the duration of your menstrual cycles and the dates of your periods. Based on past cycles, you may use this to estimate when you could ovulate.
Basal body temperature tracking
Measure your basal body temperature (BBT) every morning before getting out of bed using a specialized BBT thermometer. A slight increase in temperature can indicate that ovulation has occurred.
Cervical mucus monitoring
Observe changes in the consistency and appearance of your cervical mucus throughout your cycle. This can help you identify the fertile window when you’re most likely to conceive.
IV. Common Menstrual Cycle Concerns
A. PMS (Premenstrual Syndrome)
Symptoms
Physical, emotional, and behavioral symptoms that appear in the days before menstruation are referred to as premenstrual syndrome (PMS). Bloating, breast discomfort, mood fluctuations, irritability, exhaustion, and food cravings are typical symptoms. Some women have modest pain from PMS symptoms, while others experience more severe symptoms that interfere with everyday living.
Management and treatment
Over-the-counter painkillers, hormonal birth control, and lifestyle modifications including regular exercise, a healthy diet, and stress management strategies may all be used to treat PMS. Consult a medical expert for an assessment and treatment advice if your symptoms are severe or persistent.
B. Irregular cycles
Causes
Hormonal imbalances, stress, severe weight changes, certain medicines, and underlying medical issues like polycystic ovarian syndrome (PCOS) or thyroid disorders can all contribute to irregular menstrual periods. It’s normal for cycles to be irregular during adolescence or perimenopause, but persistent irregularities may warrant medical attention.
When to seek medical help
If you experience consistently irregular cycles, missed periods, unusually heavy or prolonged bleeding, or severe pain, it’s essential to consult a healthcare professional for evaluation and appropriate treatment.
C. Amenorrhea (absence of menstruation)
Primary and secondary amenorrhea
Amenorrhea refers to the absence of menstruation. Primary amenorrhea occurs when a girl has not started menstruating by age 15. Secondary amenorrhea occurs when a woman who has previously menstruated experiences an absence of periods for three months or longer.
Causes and treatment
Amenorrhea may be brought on by hormonal imbalances, certain drugs, intense exercise, food disorders, pregnancy, nursing, menopause, and other medical issues. Depending on the underlying reason, amenorrhea may be treated with hormone treatment, a change in lifestyle, or by taking care of any underlying medical concerns.
D. Dysmenorrhea (painful menstruation)

Primary and secondary dysmenorrhea
The medical word for uncomfortable menstrual cramps is dysmenorrhea. While secondary dysmenorrhea is brought on by an underlying medical condition like endometriosis, uterine fibroids, or pelvic inflammatory disease, primary dysmenorrhea is brought on by regular uterine contractions during menstruation.
Causes and treatment
The underlying cause of the discomfort and the degree of dysmenorrhea are factors in treatment. Over-the-counter painkillers, hormonal birth control, and lifestyle modifications including exercise, heat treatment, and relaxation techniques can all assist manage discomfort in patients with primary dysmenorrhea. It’s critical to treat the underlying issue in people with secondary dysmenorrhea with the assistance of a medical practitioner.
E. Heavy menstrual bleeding

Causes
Menorrhagia, or excessive menstrual bleeding, can be caused by endometriosis, uterine fibroids or polyps, hormonal imbalances, bleeding disorders, or certain drugs. Prolonged or excessive bleeding can lead to anemia and negatively impact daily life.
Treatment and management
Treatment for heavy menstrual bleeding may include hormonal birth control, medications to regulate bleeding, or surgical interventions in more severe cases. If you experience heavy bleeding, consult a healthcare professional for proper evaluation and treatment.
V. Menstrual Cycle and Fertility
A. Menstrual cycle and conception
By pinpointing your fertile window—the time throughout your cycle when you are most likely to conceive—understanding your menstrual cycle might help you maximize your chances of pregnancy. Ordinarily, the fertile window lasts six days, concluding on the day of ovulation. It’s significant to remember that sperm may remain alive for up to five days in the female reproductive system. The probability of conception can also be increased by having sexual activity in the days before ovulation.
B. Tracking fertility
There are several methods for tracking your fertility and identifying your fertile window, including:
Calendar tracking
You may determine when you are most likely to ovulate and become pregnant by keeping note of the duration of your menstrual cycles. Ovulation usually occurs around 14 days before the start of your next period.
Ovulation predictor kits (OPKs)
These kits detect the LH surge in urine, signaling that ovulation is likely to occur within 24-48 hours. Using OPKs can help you time intercourse to increase the chances of conception.
Cervical mucus monitoring
As mentioned earlier, monitoring changes in cervical mucus can help you identify your fertile window. Fertile cervical mucus is typically straightforward, slippery, and stretchy, resembling raw egg whites.
Basal body temperature tracking
Tracking your BBT can help you identify a pattern of temperature shifts that indicate ovulation has occurred. A sustained temperature increase usually signals that ovulation has taken place.
C. Fertility challenges and treatments
If you’re having problems becoming pregnant, it’s crucial to consult with a healthcare professional so they can evaluate your fertility and go through your treatment options. A number of factors, including hormonal imbalances, structural issues, old age, or underlying medical conditions, might prevent conception. Treatments may include lifestyle changes, medications, assisted reproductive technologies (ART), or surgery, depending on the cause of the fertility challenges.
Also Read: PCOS and Pregnancy – Fastest Way to Get Pregnant with PCOS
VI. Menstrual Hygiene and Self-Care
A. Menstrual hygiene products
For comfort, cleanliness, and general reproductive health during menstruation, proper menstrual hygiene is crucial. Various menstrual hygiene products are available to suit individual preferences and needs:

Pads
Pads are absorbent materials worn in underwear to collect menstrual blood. They come in different sizes, absorbencies, and materials, such as disposable or reusable cloth pads.
Tampons
Tampons are absorbent cylinders inserted into the vagina to absorb menstrual blood before it exits the body. To decrease the danger of toxic shock syndrome (TSS), they should be replaced every 4 to 8 hours and come in a variety of sizes and absorbencies.
Menstrual cups
Menstrual cups are reusable, flexible cups made from silicone, rubber, or latex inserted into the vagina to collect menstrual blood. They can be worn for up to 12 hours by emptying, cleaning, and reinserting.
B. Pain relief and self-care
Managing menstrual pain and discomfort is essential for maintaining well-being during your period. Various methods can help alleviate pain and promote relaxation:
Medications
Two over-the-counter medicines, ibuprofen and naproxen, may help reduce swelling and cramping related to menstruation. Always take your prescriptions as prescribed, and see your doctor if you have any concerns about whether a drug is appropriate for you.
Also Read: Period pains: Can anti-inflammatory drugs help?
Heat therapy
Applying heat to the lower abdomen can help relax the uterine muscles and alleviate cramps. Consider using a heating pad, hot water bottle, or warm towel for relief.
Relaxation techniques
Deep breathing exercises, meditation, or gentle stretching can help reduce stress and alleviate menstrual discomfort.
C. Nutrition and exercise
Your menstrual cycle and general reproductive health can benefit from maintaining a balanced diet and doing regular exercise:
Dietary recommendations
Eating a nutrient-rich diet that includes whole grains, lean protein, healthy fats, fruits, and vegetables may help to lessen the symptoms of menstruation. Limiting caffeine, salt, and processed foods may help to reduce bloating and mood swings.
Benefits of physical activity
Exercise on a regular basis helps ease mood swings, ease period cramps, and generally enhance wellbeing. Strive to do two or more days of muscle-strengthening activities per week in addition to at least 150 minutes of moderate-intensity aerobic activity or 75 minutes of vigorous-intensity aerobic exercise every week.
Also Read: Parenting Tips for first-time mommies– Things you should know
VII. Conclusion
The key to reproductive health and self-care is to comprehend your menstrual cycle. You may make wise choices regarding your health, fertility, and menstrual hygiene by being familiar with the many menstrual cycle phases, the hormones involved, and differences in cycle duration.
It’s critical to be aware of typical menstrual cycle problems and to get medical attention if you have severe symptoms or chronic anomalies. Menstrual cycles and general wellbeing can be enhanced by healthy eating, consistent exercise, and stress management.
Take control of your reproductive health by arming yourself with information of your menstrual cycle. Keep in mind that every woman’s cycle is different, and that sustaining your health and wellbeing depends on your ability to recognize your body’s own patterns and demands.



